Our research projects
This section introduces the projects of the Developmental & Cellular Biology group
-
Duration:
December 2024 – December 2028
-
Funding source:
Interreg North-West Europe
-
Researchers:
Noemi Asfogo, Matthieu Gobin, Jens C. Schwamborn
-
Partners:
The project is led by BioRegio STERN (DE) with a consortium of 10 partners representing 6 countries of the North-West Europe region (LU, DE, IE, NL, FR, BE).
-
Description:
The DVB team is part of STEP4NAMs, a recently awarded Interreg North-West Europe (NWE) region project.

STEP4NAM consortium meeting
The project’s objectives are to:
- Reduce the obstacles in NAM (novel alternative methods) usage and uptake in the (Bio)Pharma & MedTech sectors through an in depth analysis on the national/regional conditions within participating NWE regions
- Facilitate the future uptake of NAMs through the implementation of four pilot studies demonstrating and testing a diverse set of NAMs as best practices of validation: Organ-on-chip, organoids, digital twin & bioprinting/bench-top simulations ultimately resulting into a Validation Manual for NAM users and developers
- Educate stakeholders along the value chain of NAM development through a tailored three pillar training & support programme, providing the necessary knowledge, guidance and experience in the use/development of NAMs
Specifically, the DVB team will be the driver of Pilot IV that aims to showcase the potential of PD-specific brain organoids to predict the failure of promising PD drug candidates that were effective in pre-clinical studies but failing in human clinical trials. The aim is to give the opportunity to at least 4 SMEs/companies to test their failed compound in our PD midbrain organoid model and thus confirm or refute the observed clinical trial results. This will be achieved by analysing PD-disease phenotypes in the midbrain organoids using patient-derived and control cell lines. The outcome will serve as demonstration that organoids for pre-clinical testing benefit biotech SMEs and Big Pharma by offering a cheaper and efficient testing platform.
Total budget: 6.332.365,47€ (UL budget: 736.939,02€) – EU funding: 3.799.419,27€
Social media accounts: LinkedIn
-
Project details (PDF):
-
Duration:
-
Funding source:
-
Researchers:
-
Partners:
-
Description:
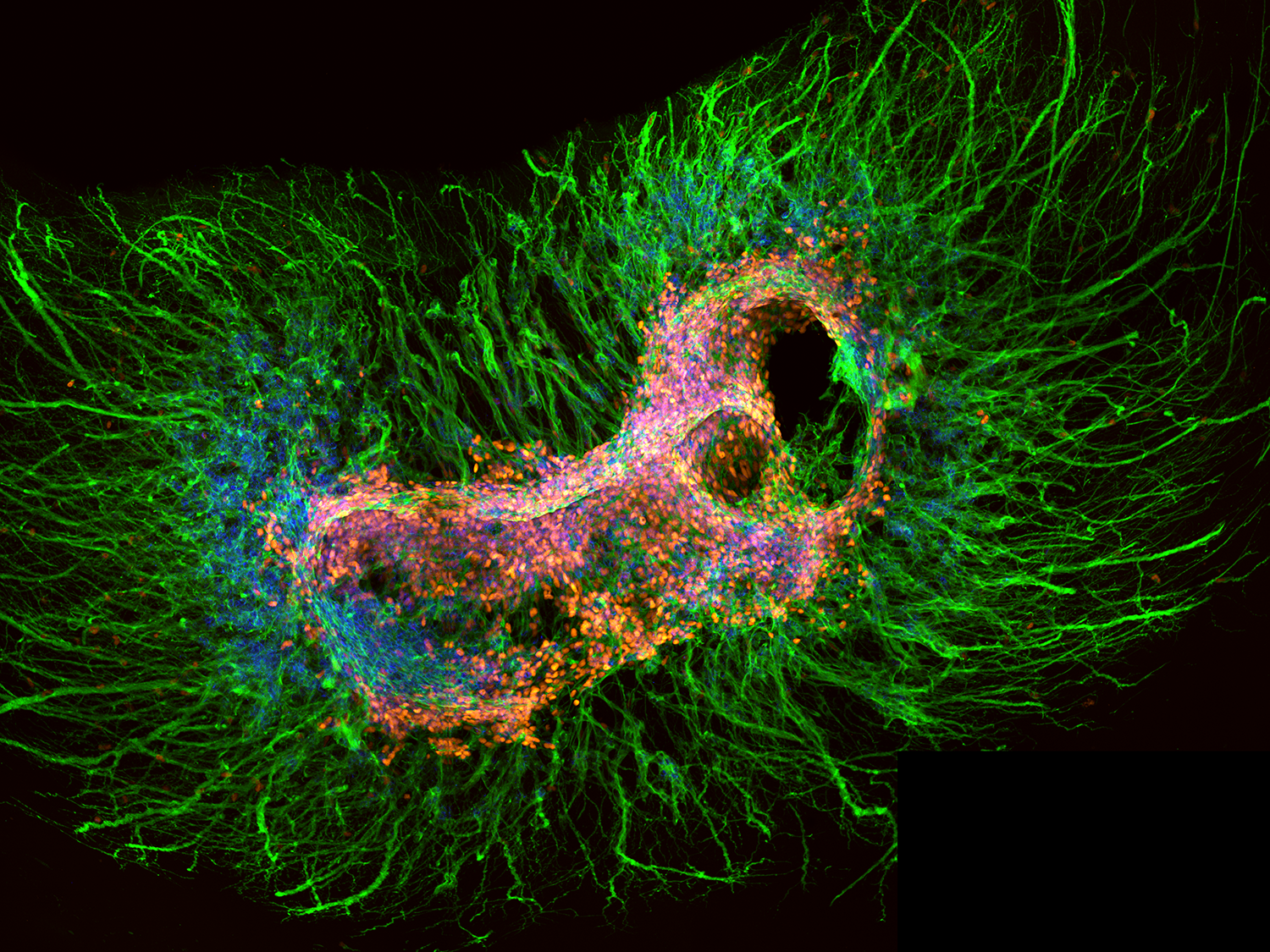
Parkinson’s disease is a progressive neurological disorder. It is the second most common neurodegenerative disease after Alzheimer’s disease. Currently about seven million people are affected. A major disadvantage in 2D cell cultures of dopaminergic neurons as well as in midbrain organoids is the fact that in these models the dopaminergic neurons mainly form synapses with other dopaminergic neurons, while in vivo they form synapses with GABAergic spiny projection neurons in the striatum. Since one of the key proteins in the PD pathogenesis, alpha-Synuclein, is a synaptic protein, we hypothesize that the inadequate modeling of synaptic connections in current in vitro models reduces their predictively for disease-associated processes. Hence, we here follow the objective to develop a novel in vitro model, consisting of connected midbrain and striatum organoids (assembloid), recapitulating synaptic connections of midbrain dopaminergic neurons that are similar to those developed in vivo. We expect that, when we derive these assembloids from PD patient specific stem cells, alterations in these synaptic connections can be detected. Furthermore, we speculate that these synaptic alterations precede disease-associated processes like the loss of dopaminergic neurons. We assume that higher levels in alpha-Synuclein leads to alterations in synaptic number and/or function. These might be either increased or decreased. In any case, if we detect synaptic alterations, rescuing them might have the potential to also rescue dopaminergic neuron loss. Since synapse function and stabilization largely depends on the activity of growth factors like BDNF, GDNF, IGF and NGF, we suggest that modulating growth factor levels might also rescue other alterations, e.g. in synapse function and dopaminergic neuron number.
-
Project details (PDF):
-
Duration:
-
Funding source:
-
Researchers:
-
Partners:
-
Description:
Parkinson’s Disease (PD) is a neurodegenerative disease characterised by a progressive loss of striatal dopaminergic projecting neurons of the midbrain’s substantia nigra. Alpha-Synuclein (a-Syn), encoded by the SNCA gene, is the main component of the Lewy bodies that accumulate
in the brains of people with PD. In fact, SNCA together with other genes such as LRRK2, GBA, PRKN, PINK1, PARK7, belong to the group of genetic factors associated with the disease. However, most of the patients do not show an obvious genetic cause, designated as idiopathic (sporadic) cases. Several studies implicate aging and neuroinflammation as main risk factors for the disease onset. However, the exact mechanisms underlying neuronal degeneration and PD etiology remain unclear, due to the lack of human models recapitulating all disease features. In this study, we aim to apply state-of the art stem cell and organoid technology to model the disease microenvironment in vitro using induced pluripotent stem cells (iPSC) derived from genetic and sporadic PD patients, and use these models as a platform to study the relationship between PD main risk factors: aging, neuroinflammation and a-Syn as a paradigmatic genetic example. For this purpose, we will generate and comprehensively assess i) axotomised midbrain-forebrain assembled 3D organoids, ii) a neuroinflammatory model by confronting microglia to midbrain-like organoids and iii) a paired 2D-3D culture system. Moreover, to better recapitulate the disease pathophysiology, we will induce aging in all these models by overexpressing Progerin, a mutated protein shown to increase pathophysiological hallmarks of PD in iPSC-derived models. Comprehensive live imaging, transcriptomics and proteomics will be performed as functional read-outs. By establishing novel functional organoid models for PD, we expect to recapitulate nigro-striatal microenvironment as a means to bridge the gap between current model system and human brain pathology. This will allow us to directly correlate the relation between key PD hallmarks and to decipher early crucial pathological events that will help to understand the disease and provide a robust basis for the development of drug validation and screening. Moreover, the analysis will allow us to find novel PD biomarkers that may help to predict the development of the disease at early stages using easily accessible biosamples.
-
Project details (PDF):
-
Duration:
-
Funding source:
-
Researchers:
-
Partners:
-
Description:
In recent years, a growing number of studies demonstrated the relevance of understanding the molecular underpinnings of disease-disease associations, or so-called comorbidities, for the development of novel, and more effective therapies in various disease circumstances. Here, we will focus our efforts on studying the connections between two diseases of growing relevance in our societies, with an established epidemiological connection: diabetes and Parkinson’s disease.
Parkinson’s disease (PD) is a prevalent age-associated neurodegenerative disorder affecting over 7 million affected people worldwide, and with high prevalence in the population above 60 years (about 1%). The main pathological characteristic of PD is the degeneration of dopaminergic neurons in the substantia nigra of the midbrain, giving rise to typical clinical features such as motor symptoms including rigidity, bradykinesia, tremor and postural instability. Generally, these late-stage manifestations are preceded, in a prodromal stage, by non-motor symptoms like hyposmia, constipation, sleep disturbances and depression. Additionally, a key neuropathological characteristic of PD is the presence of the so-called Lewy pathology, which consists of intra-neuronal (Lewy bodies) and intra-neurite (Lewy neurites) protein aggregations, mainly consisting of the protein alpha-synuclein (aSyn). Defects in energy metabolism, particularly including mitochondrial dysfunctions, are a potential cause for PD. Importantly, metabolic alterations are present at early stages of PD, and have been mechanistically associated with the pathological accumulation of aSyn. For example, lipid metabolism alterations, and sugar dyshomeostasis (e.g. diabetes) are known to modulate the aggregation of aSyn, which likely starts 20-30 years before the onset of motor features.
Diabetes is a metabolic condition characterized by chronic hyperglycemia leading to deregulated glucose homeostasis that initiates a multitude of complications at multiple sites of the human organism, including diabetic nephropathy and neuropathy if left untreated. In 2017, more than 460 million individuals were affected by diabetes. This constitutes is about 6.3% of the world’s population or 6.000 cases per 100.000. This number will increase to about 7.000 cases per 100.000 by 2030. The vast majority of patients are diagnosed with type 2 diabetes (T2D), a progressive condition in which the body becomes resistant to the normal effects of insulin (storing of intravenous glucose in the tissue) and/or gradually loses the capacity to produce enough insulin in the pancreas, thereby causing hyperglycemia. This project will focus on the interplay between T2D and PD, given our limited understanding of the molecular underpinnings of the association between the two conditions.
Importantly, alterations in sugar metabolism, such as those observed in T2DM, can lead to the age-associated accumulation of glycated proteins. In fact, glycated hemoglobin is routinely used as a clinical marker of diabetes in the blood. Glycation is a non-enzymatic, age-associated posttranslational modification (PTM) that can tremendously impact on the biology of the proteins affected and of the cells/tissues where they accumulate in the form of advanced glycation end products (AGEs). These AGEs can trigger, for example, the activation of microglial cells and, therefore, neuroinflammation. In addition, a variety of T2DM related stressors, e.g. hyperglycemia, dyslipidemia, and glucose oscillations, foster a number of pathways ultimately leading to chronic, low-grade inflammatory responses and loss of proteostasis. Indeed, glucose and lipids promote the accumulation of senescent cells, the dysregulation of cellular anti-oxidant systems, increased oxidative/nitrosative stress, and cause endoplasmic reticulum (ER) stress and other proteostasis deffects.
-
Project details (PDF):
-
Duration:
-
Funding source:
-
Researchers:
-
Partners:
-
Description:
Novel micro-engineered in vitro models have been developed to mimic key functions of human organs. These so-called organ-on-chips (OoC) recapitulate the structure and function of human organs, and are particularly important for scientific research that is underlying our knowledge base of diseases and for the pre-clinical development of novel therapeutics. However, the application of these models has its limitations as they do not mimic the complexity and functioning of complete organ systems. Connectivity between cells and the linkage between different components of organ systems is essential in studying complex conditions such as neurodegenerative diseases. These diseases form a major challenge for the scientific community and are associated with a heavy burden on society and the global healthcare systems. To effectively grasp the complexity of neurodegenerative disorders, the CONNECT consortium develops the next level in vitro model systems for the nervous system and puts it firmly on the map. The project acts at the convergence of a multitude of disciplines including nanofabrication, microfluidics, stem cell technology, tissue engineering and advanced imaging. The successful completion of this high risk-high gain project will enable for the first time to study a complete organ system and deliver a viable paradigm for future technology to study connectivity in the nervous system. The proposed work in this project offers a unique opportunity to culture individual nervous system components and connect them in a single “smart” microfluidic chip (CONNECT platform), forming an elementary three compartment model from the central nervous system (CNS) to the peripheral nervous system (PNS). As Proof-of-Principle, CONNECT will demonstrate the feasibility of this system model in Parkinson’s Disease. This provides CONNECT with novel insights, thereby paving the way for future development of therapeutic strategies.
-
Project details (PDF):
-
Duration:
-
Funding source:
-
Researchers:
-
Partners:
-
Description:
In this project, we will develop a novel generation of bio-organic computer chips which are based on the exceptional computing capacities of the human brain. In contrast to a classical CPU, we envision the development of a biological processer unit (BPU) that is based on the use of brain organoids that are integrated in an advanced organ-on-a-chip system containing embedded laser waveguides and electrical actuators. A single human brain has an estimated storage capacity of about 2.800 TB and is 100.000 times more energy efficient than a traditional computer. For comparison, the AI system DeepMind/AlphaGo consumed as much as 1MW in an internationally advertised Go challenge match versus the best human player, whose total energy expenditure for playing was only 20W. Considering the enormous energy demands of today’s computers and especially in AI related computing, brain organoid based computers will be a major game changer when it comes to developing energy efficient and climate friendly technologies, with similar or higher computing performances. Our target is to initiate computing power through biological processes to demonstrate the capability of brain organoids as computers. This will be achieved by exploiting the inherent ability of neurons to recognise and transmit electrical signal patterns to solve mathematical problems by implementing various on-chip stimulation and training routines. Our priority is to establish the technological foundations of a BPU capable of solving easy mathematical or logic problems. Ultimately, we envision to fully take advantage of the inherent energy efficiency of the human brain and ultimately to see our BPU evolve and develop some indication of intelligence. The presented radical innovation is that for the first time in vitro generated human brain organoids will be used for conducting intelligence-requiring tasks thus representing a conceptually new approach, advancing from Artificial Intelligence to “Organoid Intelligence (OI)”.
-
Project details (PDF):