The project at a glance
-
Start date:01 Mar 2022
-
Duration in months:48
-
Funding:Luxembourg National Research Fund (FNR)
-
Principal Investigator(s):Elisabeth LETELLIER
About
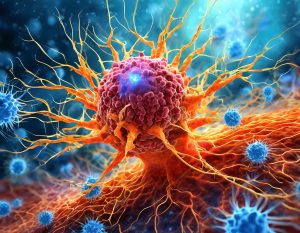
As the third most common form of cancer, colorectal cancer (CRC) is a major healthcare challenge worldwide. While public colorectal cancer (CRC) screening campaigns have yielded great success by preventing disease development through removal of precancerous lesions, many patients are still left with few effective therapeutic options as they often present with an advanced disease stage at diagnosis. Indeed, over 50% of patients are diagnosed in stages III or IV. Immune checkpoint inhibitors are a class of drugs that has changed the way we treat many cancers, but unfortunately, they show little effectiveness for the majority of CRC patients. Indeed, CRC tumors are often described as immunologically cold, being unable to elicit and sustain effective immune responses. The complex interplay between the immune and stromal compartments of the tumor microenvironment (TME) play a key role in tumor development and the above-mentioned immune escape. Within the TME, a stromal cell type known as cancer associated fibroblasts (CAF) have been emerging as a key player in determining patient outcomes and therapeutic efficacy. There’s been a growing body of knowledge on the interactions between CAF and immune cells, with CAF being shown to have a profound effect on both the makeup and functional properties of the immune compartment in the TME. Type I interferons (IFN-I) are a family of cytokines that are known to have a multitude of immunomodulatory effects. In the tumour microenvironment, high levels of IFN-I are reported to favour the development of a tolerogenic niche, with IFN-I being reported to induce PD-L1 expression multiple TME cell types, as well as causing increased proliferation and maintenance of immunosuppressive regulatory T-cells. Sustained IFN-I signalling has been proposed as a resistance mechanism to PD-L1 blockade based immune checkpoint inhibition therapies. Recent in-vitro studies have further shown that blocking of IFN-I could eliminate CAF dependant chemoresistance in breast cancer, however in-vivo data and information on the impact of this pathway in CRC and immunotherapy are major unexplored areas with promising implications for future treatments. In single cell RNA sequencing datasets of patient-derived CRC tissue, we observed that cancer associated fibroblasts expressed significantly higher levels of IFN-I receptors and downstream targets then normal fibroblast from outside the cancer margin. Tumors expressing high levels of IFN-I showed significantly reduced overall survival and were associated with a tolerogenic immune signature. They presented elevated levels of M2 macrophage polarization, T-cell exhaustion and inhibitory checkpoint molecule PD-L1. Further in-vitro experiments showed that CAF increased their PD-L1 surface expression when treated with IFN-α. Based on the reported immunomodulatory functions of IFN-I in the TME and on the supporting preliminary findings discussed above, we would like to highlight IFN-I signalling in CAF as a major unexplored area with promising implications for improving treatment responses. By using a combination of innovative in-vitro an in-vivo techniques as well as our internal collection of patient CRC biospecimens, we will investigate how IFN-I sensitive CAF shape the tumor immune microenvironment and their effect on chemo- and immunotherapy resistance. First, we will further characterize IFN-I sensitive CAF through a combination of bioinformatic and molecular approaches, by identifying surface markers expression patterns and differentially expressed signalling pathways. Second, we will investigate the mechanisms by which IFN-I activated CAFs influence cancer and immune cells of the TME via a variety of advanced in-vitro proliferation, invasion and co-culture assays. Finally, we will validate our findings in in-vivo preclinical models of CRC using stromal specific knockouts of IFN-I receptors. Immune phenotyping and treatment response rates to common immuno- and chemotherapy treatment plans will give valuable insight as to the clinical potential of stromal directed therapies targeting IFN-I signalling.
Organisation and Partners
- Department of Health, Medicine and Life Sciences
- Faculty of Science, Technology and Medicine (FSTM)
- Molecular Disease Mechanisms
Project team
-
Elisabeth LETELLIER